A bicornuate uterus is a uterine anomaly that is present from birth, where the uterus has a unique heart-shaped structure instead of the normal pear shape.
A bicornuate uterus is a rare uterine malformation that occurs when the Mullerian ducts don’t fuse normally during embryogenesis. It’s also known as a heart-shaped uterus because the top of the uterus dips inward at the middle.
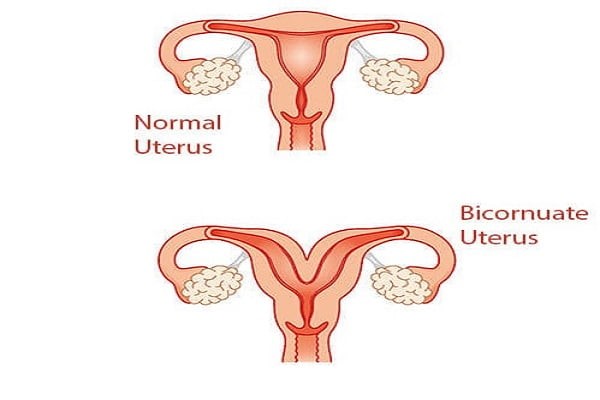
Typically, a non-pregnant uterus measures about 3 inches in length, 2 inches in width, and 1 inch in depth, expanding during pregnancy. In a bicornuate uterus, there are two connected cavities, whereas a standard uterus has one. At the top of the uterus, in the fundus area, there is a distinct indentation that gives rise to this heart-like shape, with projections or horns extending towards the fallopian tubes. The condition is relatively rare, affecting roughly one in every 200 women, many of whom are unaware of the abnormality until they become pregnant.
Symptoms can vary; some individuals may not experience any, while others might encounter:
- Multiple miscarriages
- Vaginal bleeding that deviates from the normal pattern
- Discomfort or pain in the abdominal region
- Painful Intercourse
- Menstrual periods accompanied by pain
When such symptoms are present, it is important to seek medical advice. Diagnostic imaging such as ultrasound can confirm the presence of a bicornuate uterus.
The development of a bicornuate uterus occurs during fetal life due to atypical fusion of the paramesonephric ducts. This creates a double-projection, heart-shaped uterus, which is not preventable because it’s a congenital issue.
There are other kinds of uterine anomalies – the unicornuate uterus, which is smaller, and the septate uterus, which has a wall or septum dividing it into two parts. In comparison on an imaging test, a septate uterus looks round on top and typically can be corrected with a surgical procedure known as hysteroscopic surgery.
While uterine malformations are uncommon, they can be linked to fertility issues, pregnancy loss, growth restrictions of the foetus, premature births, and higher caesarean section rates. Nevertheless, some women with these anomalies experience normal reproductive outcomes.
A bicornuate uterus is diagnosed through imaging tests such as ultrasound, MRI, or a hysterosalpingogram (HSG). Occasionally, a laparoscopy might be performed for a clear and definite diagnosis.
In terms of treatment, not everyone with a bicornuate uterus will need it. However, for those who undergo repeated miscarriages, a surgical procedure called Strassman metroplasty is advised to merge the two cavities into one. The effectiveness of this surgery concerning fertility is debatable, as becoming pregnant with a bicornuate uterus may not be significantly impeded.
For fertility issues, in vitro fertilization (IVF) is another option, where fertilization occurs outside the body in a laboratory setting. Nonetheless, even after successful IVF, a caesarean delivery might be necessary.
Pregnant women with a bicornuate uterus are advised to undergo more frequent monitoring to manage risks early. While the condition does add complexity, with proper care and information, many women can successfully manage their pregnancies.
At a fertility clinic such as 9M Fertility centres in Hyderabad, Pune and Bhubaneswar, we emphasize comprehensive and empathetic care to support individuals on their path to parenthood.
